Free Do Not Resuscitate Order Form for Nevada
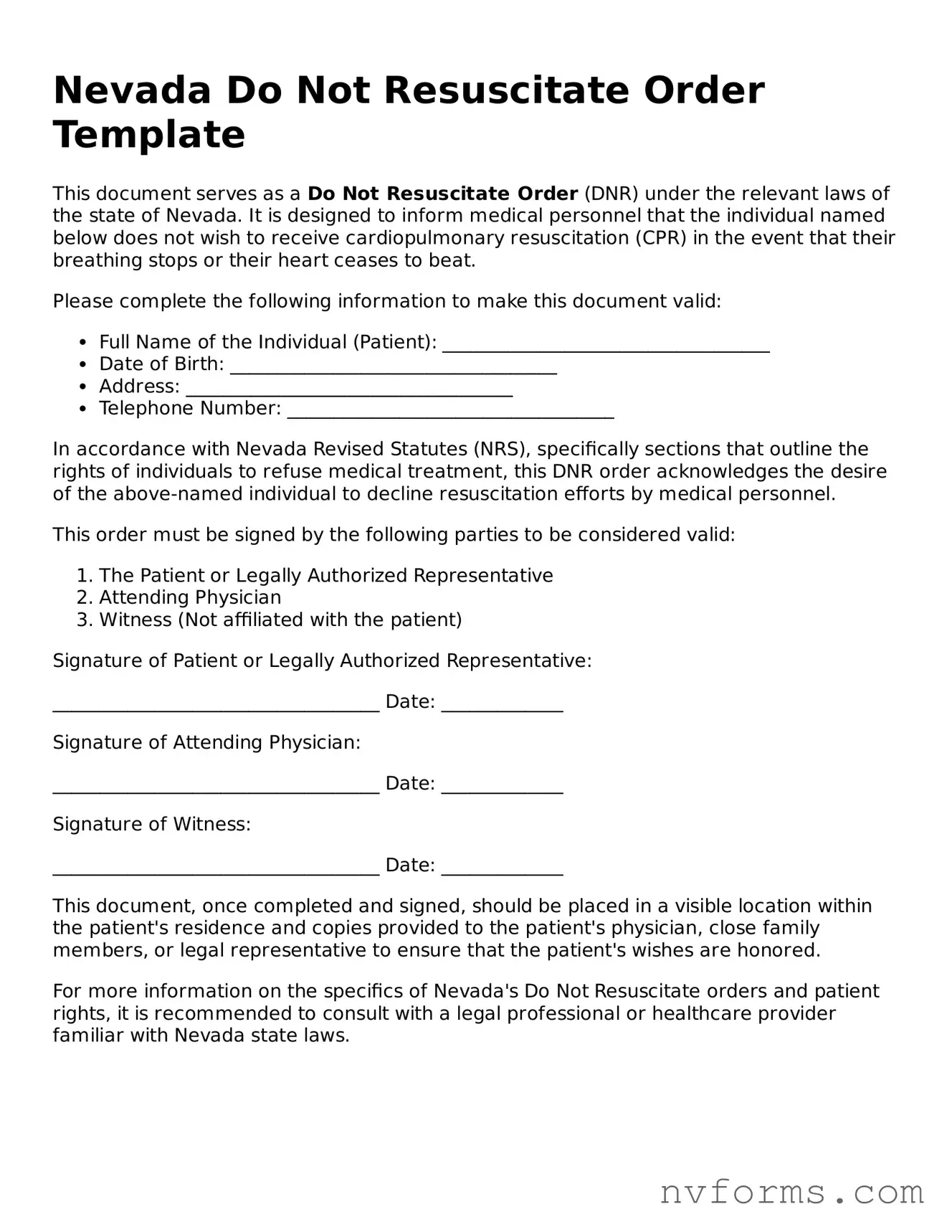
A Do Not Resuscitate Order (DNR) form in Nevada is a legal document that allows individuals to express their wish not to undergo cardiopulmonary resuscitation (CPR) or advanced cardiac life support in case they stop breathing or their heart stops beating. This form ensures that a person's choices regarding end-of-life care are respected by healthcare professionals. By completing the Nevada DNR form, individuals can communicate their healthcare preferences clearly and ensure their wishes are known in critical situations.
Launch Editor
Free Do Not Resuscitate Order Form for Nevada
Launch Editor
Launch Editor
or
⇩ Do Not Resuscitate Order File
Don’t stop now — finish the form
Finish Do Not Resuscitate Order online using an easy step-by-step flow.