Fill Out a Valid Fa 29 Nevada Template
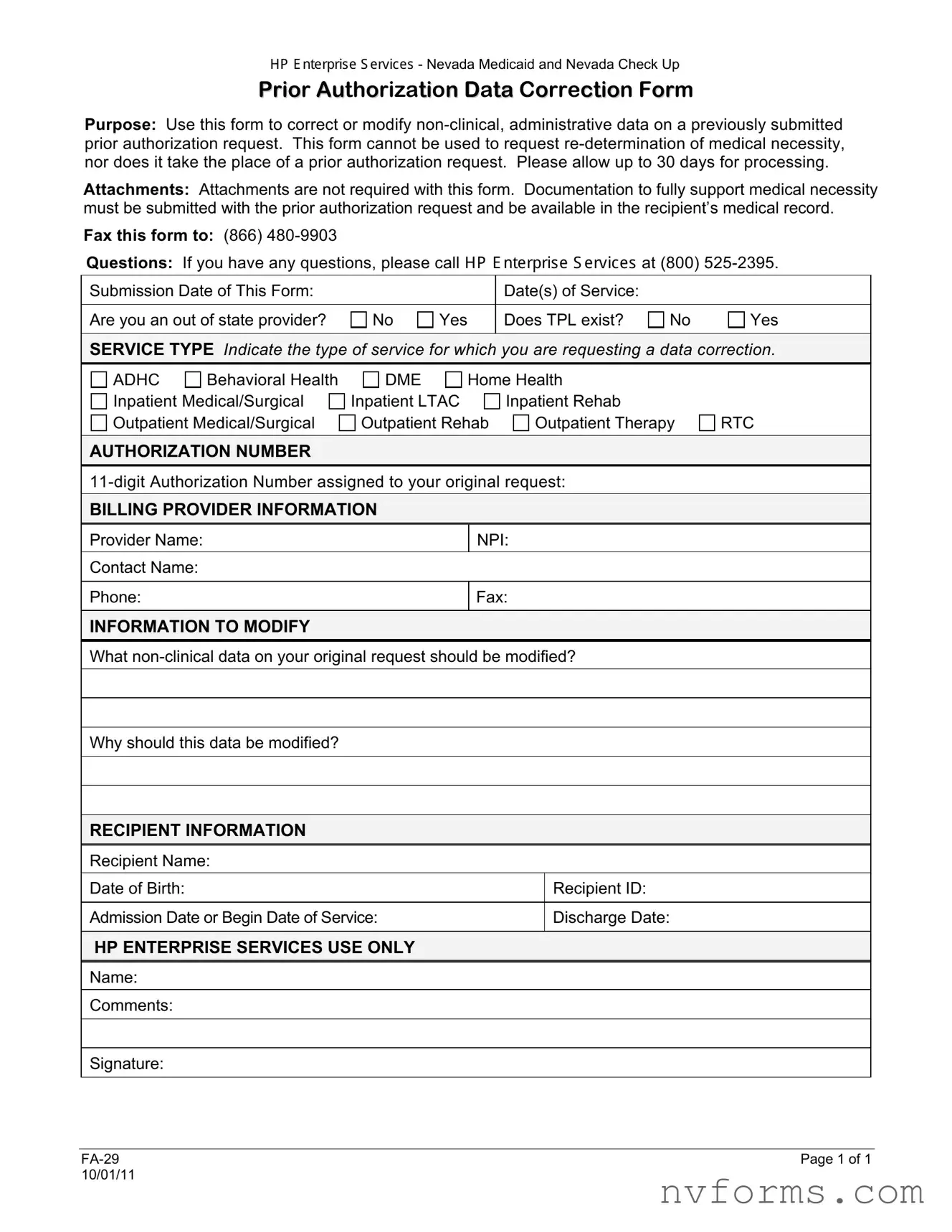
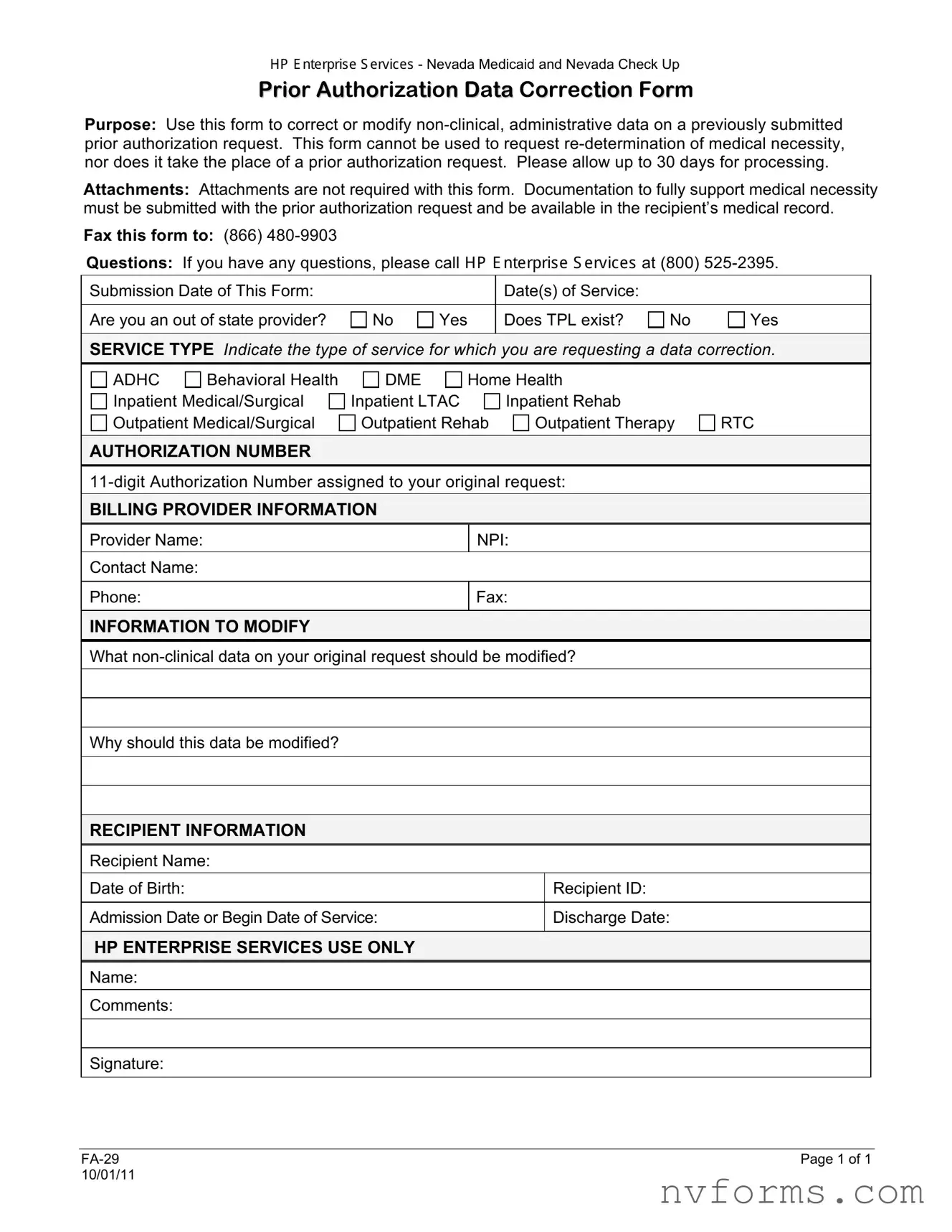
The FA-29 Nevada form serves a crucial role in the administration of Nevada Medicaid and Nevada Check Up by offering a structured way to correct or modify non-clinical, administrative data on a previously submitted prior authorization request. It is important to note that this form is not intended for the re-determination of medical necessity nor does it replace the need for a prior authorization request. Providers are advised to allow up to 30 days for the processing of these corrections, with no additional documentation required beyond what was originally submitted to support medical necessity.
Launch Editor
Fill Out a Valid Fa 29 Nevada Template
Launch Editor
Launch Editor
or
⇩ Fa 29 Nevada File
Don’t stop now — finish the form
Finish Fa 29 Nevada online using an easy step-by-step flow.