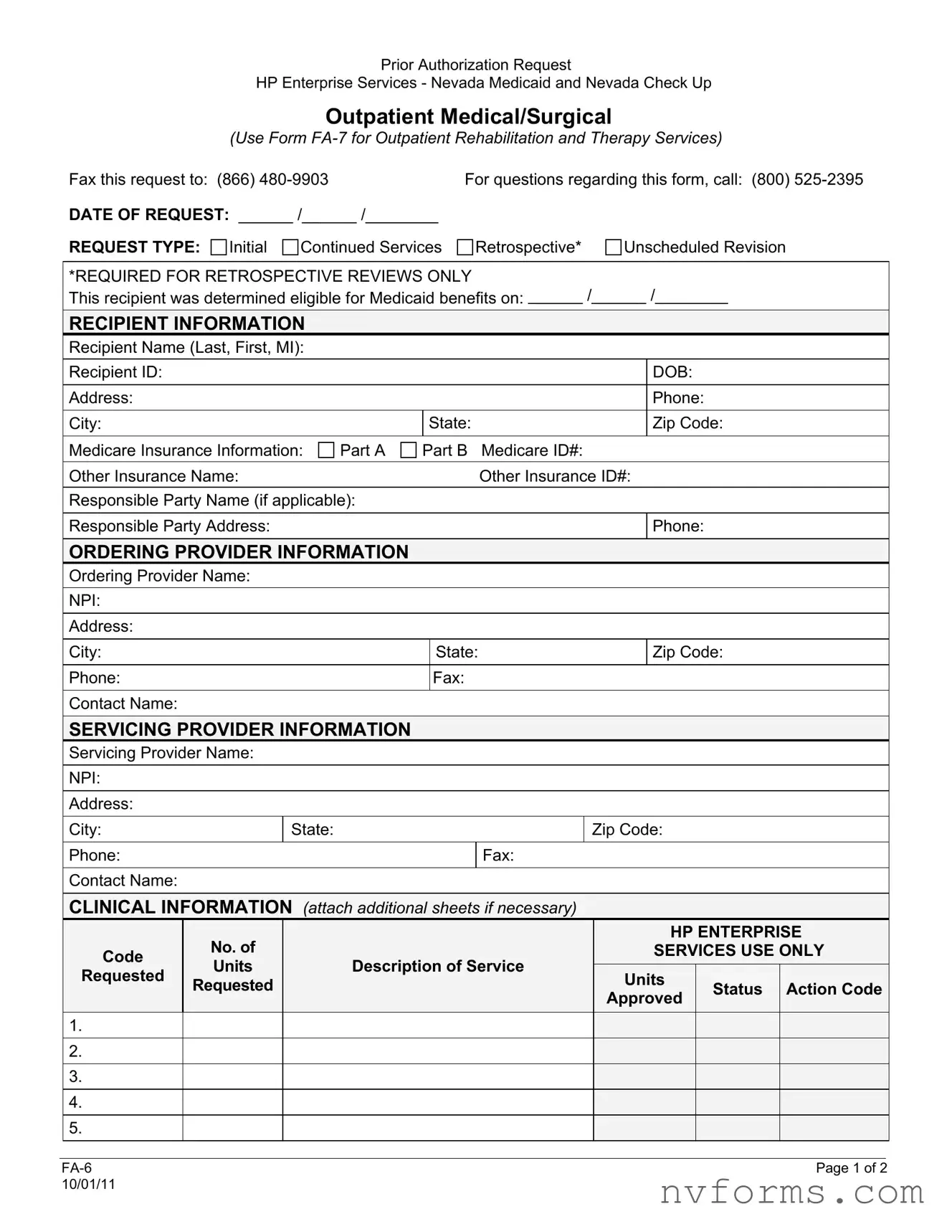
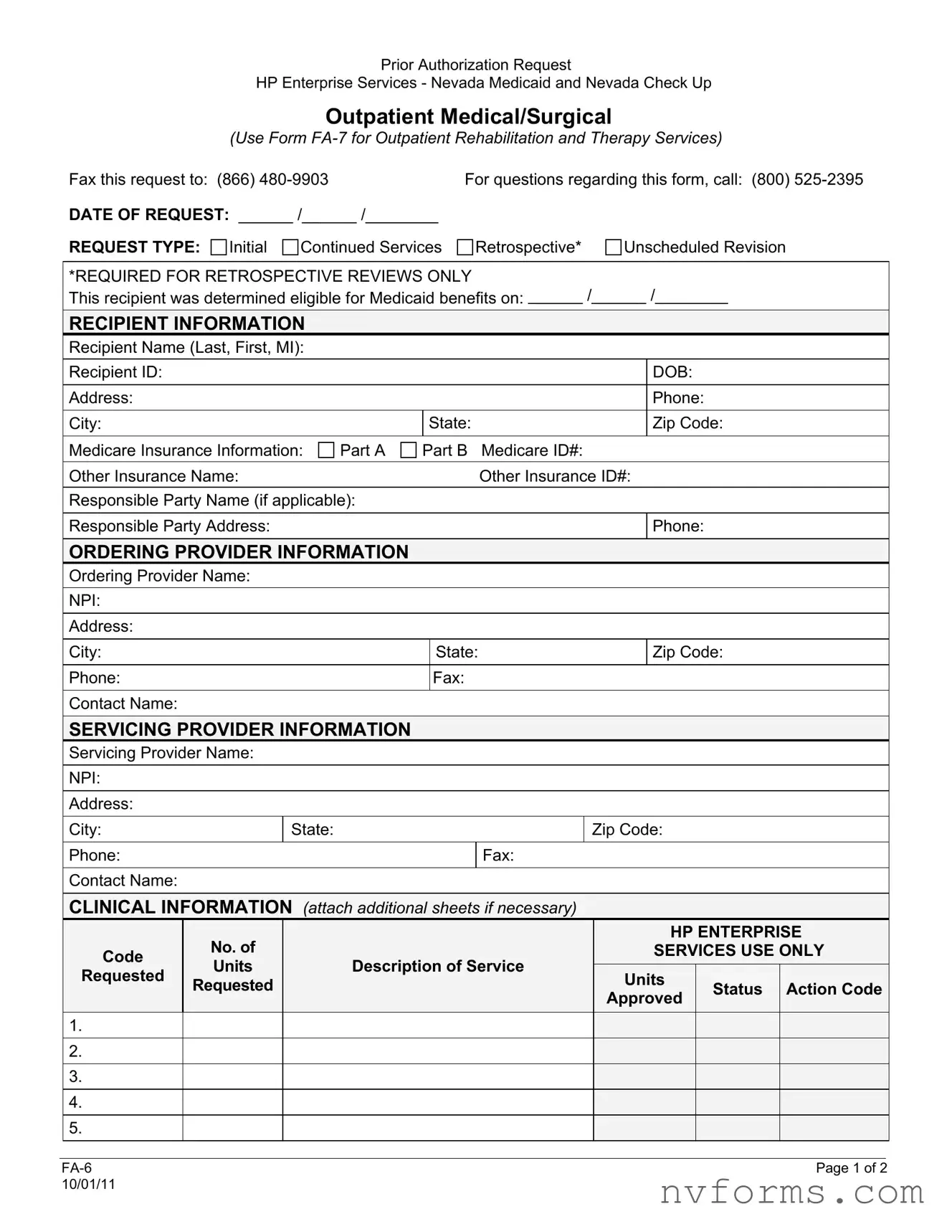
Prior Authorization Request
HP Enterprise Services - Nevada Medicaid and Nevada Check Up
Outpatient Medical/Surgical
(Use Form FA-7 for Outpatient Rehabilitation and Therapy Services)
Fax this request to: |
(866) 480-9903 |
For questions regarding this form, call: (800) 525-2395 |
DATE OF REQUEST: ______ /______ /________ |
|
|
REQUEST TYPE: |
Initial |
Continued Services |
Retrospective* |
Unscheduled Revision |
*REQUIRED FOR RETROSPECTIVE REVIEWS ONLY
This recipient was determined eligible for Medicaid benefits on: ______ /______ /________
RECIPIENT INFORMATION
Recipient Name (Last, First, MI):
Recipient ID: |
|
|
|
DOB: |
Address: |
|
|
|
Phone: |
City: |
|
State: |
|
Zip Code: |
Medicare Insurance Information: |
Part A |
Part B |
Medicare ID#: |
Other Insurance Name: |
|
|
Other Insurance ID#: |
Responsible Party Name (if applicable):
Responsible Party Address:
ORDERING PROVIDER INFORMATION
Ordering Provider Name:
NPI:
Address:
City: |
|
|
|
|
|
State: |
|
|
|
Zip Code: |
Phone: |
|
|
|
|
|
Fax: |
|
|
|
|
|
|
|
|
|
|
Contact Name: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
SERVICING PROVIDER INFORMATION |
|
|
|
|
|
|
|
|
|
|
Servicing Provider Name: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
NPI: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Address: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
City: |
|
|
|
State: |
|
|
|
Zip Code: |
|
|
|
|
|
|
Phone: |
|
|
|
|
|
|
Fax: |
|
|
|
|
|
|
|
|
|
|
Contact Name: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
CLINICAL INFORMATION (attach additional sheets if necessary) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
No. of |
|
|
|
|
|
|
|
|
|
HP ENTERPRISE |
|
|
Code |
|
|
|
|
|
|
|
|
|
|
SERVICES USE ONLY |
|
|
|
|
Units |
|
|
Description of Service |
|
|
|
|
|
|
|
|
|
|
|
Requested |
|
|
|
|
|
|
Units |
|
|
|
|
|
|
|
|
|
Requested |
|
|
|
|
|
|
|
|
|
Status |
|
Action Code |
|
|
|
|
|
|
|
|
|
|
|
|
Approved |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
3. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
4. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
5. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
FA-6 |
Page 1 of 2 |
10/01/11 |
|
|
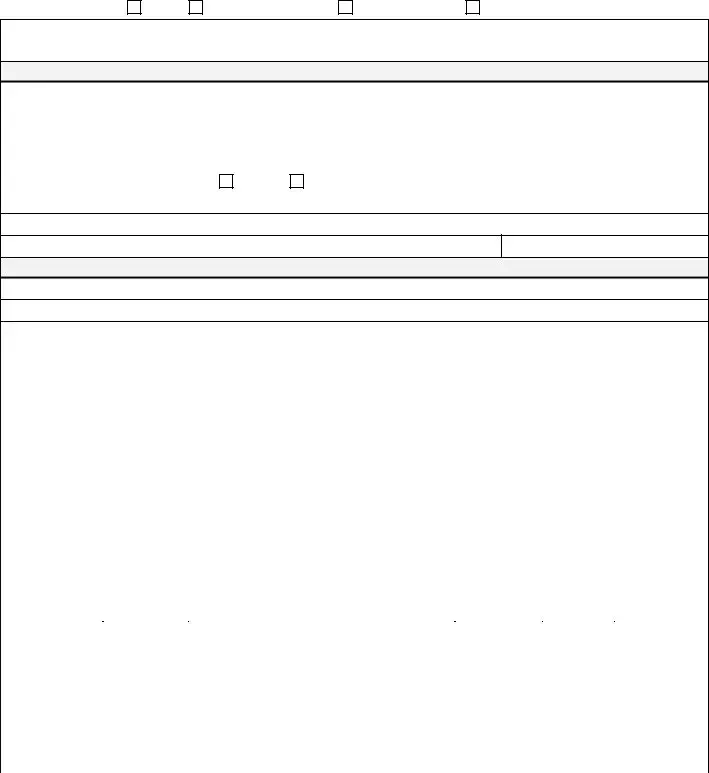
Prior Authorization Request
HP Enterprise Services - Nevada Medicaid and Nevada Check Up
Outpatient Medical/Surgical
(Use Form FA-7 for Outpatient Rehabilitation and Therapy Services)
Is the service you are requesting a hospice benefit? |
Yes |
No |
|
Are you requesting Healthy Kids (EPSDT) referral/services? |
Yes |
No |
Conditions/Symptoms (include ICD-9 codes and descriptions): |
|
|
Previous Treatment/Services (include dates):
Results of Previous Treatment/Services:
Other Clinical Information (to support medical necessity of the requested services):
HP ENTERPRISE SERVICES USE ONLY
Approved From: |
Approved Through: |
Denied From: |
Denied Through: |
Reviewer Signature: |
|
Date: |
This authorization request is not a guarantee of payment. Payment is contingent upon eligibility, available benefits, contractual terms, limitations, exclusions, coordination of benefits and other terms and conditions set forth by the benefit program. The information on this form and on accompanying attachments is privileged and confidential and is only for the use of the individual or entities named on this form. If the reader of this form is not the intended recipient or the employee or agent responsible to deliver it to the intended recipient, the reader is hereby notified that any dissemination, distribution or copying of this communication is strictly prohibited. If this communication is received in error, the reader shall notify sender immediately and destroy all information received.
|
|
|
FA-6 |
Page 2 of 2 |
10/01/11 |
|
|