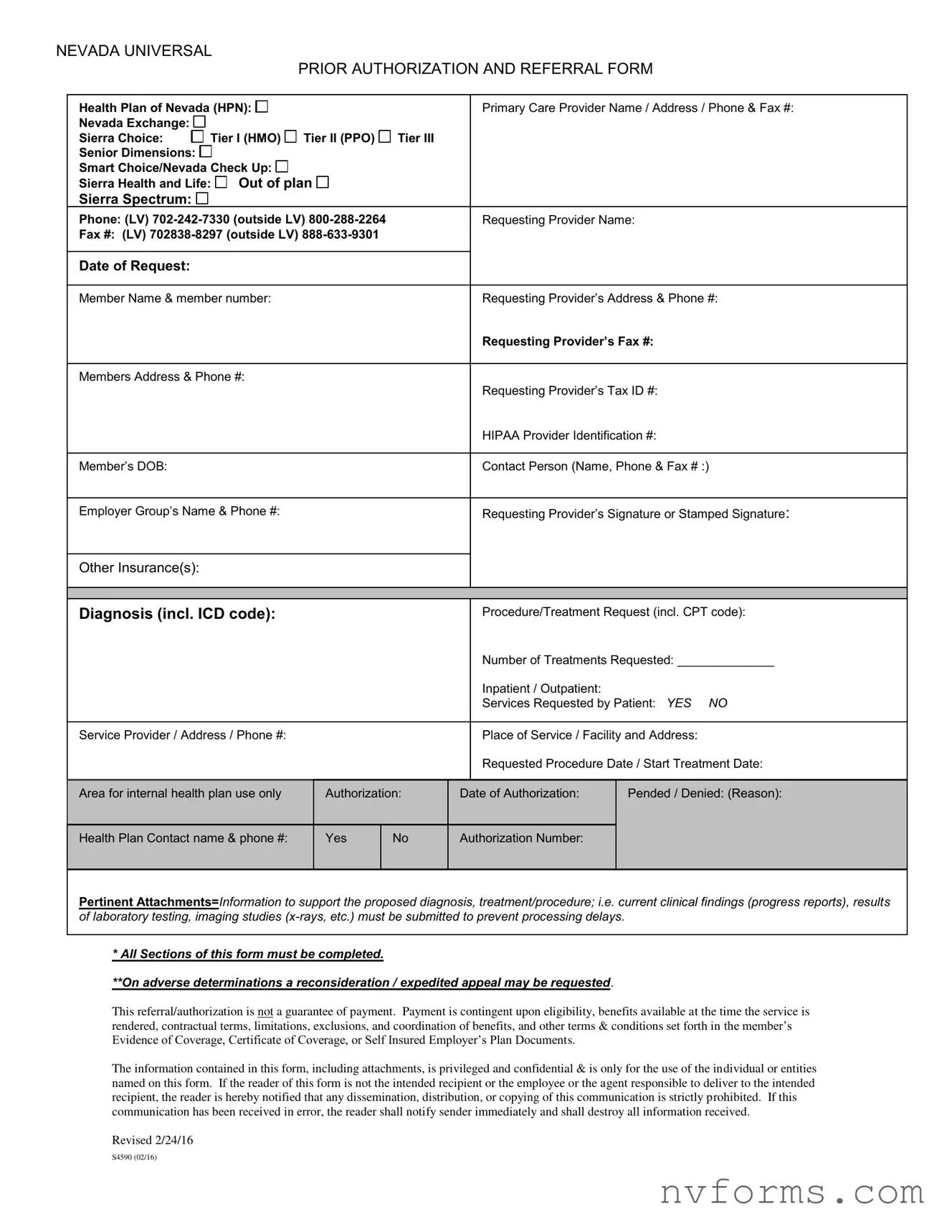
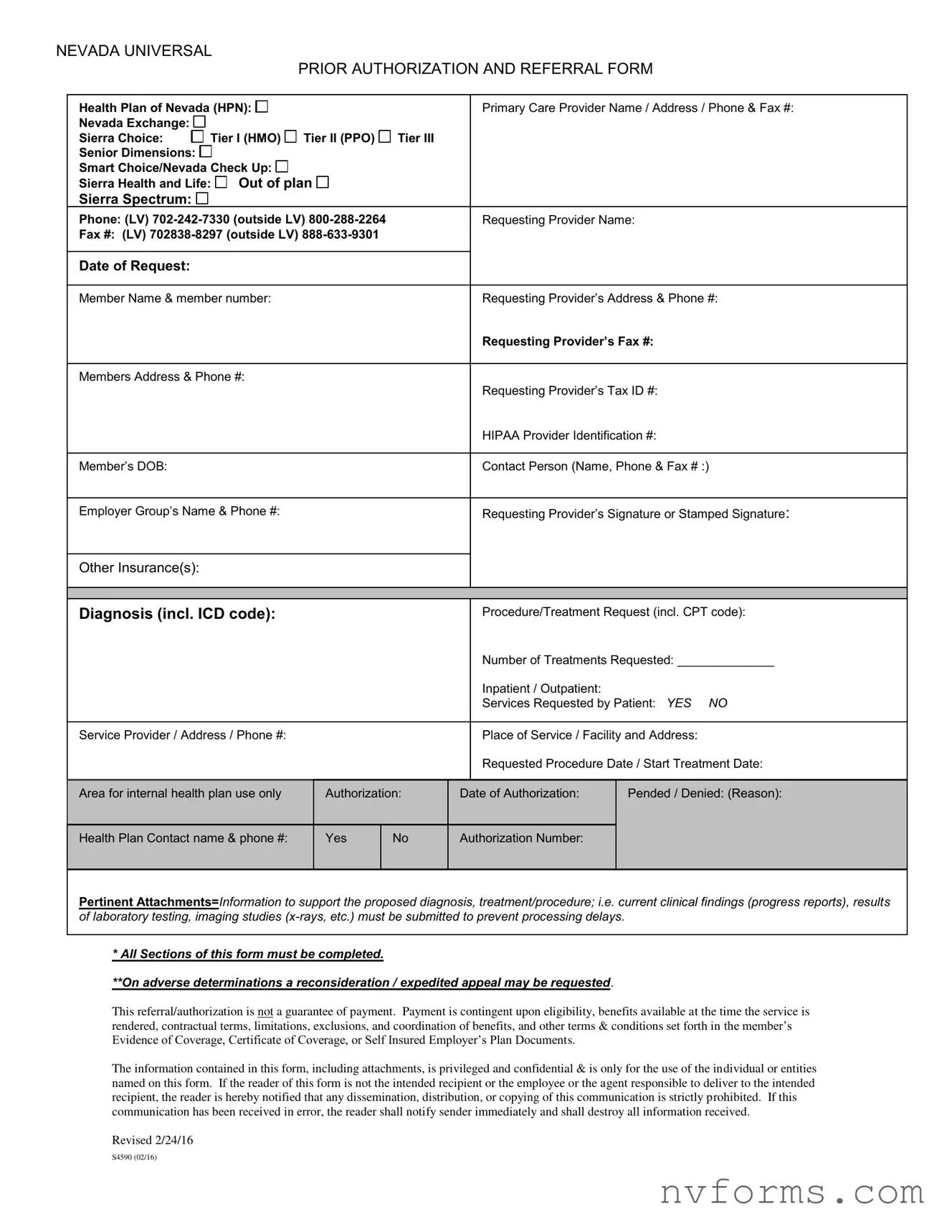
NEVADA UNIVERSAL
PRIOR AUTHORIZATION AND REFERRAL FORM
Health Plan of Nevada (HPN): |
|
|
|
|
|
|
|
|
|
|
|
|
Primary Care Provider Name / Address / Phone & Fax #: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Nevada Exchange: |
|
|
|
|
|
Tier I (HMO) |
|
|
Tier II (PPO) |
|
Tier III |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Sierra Choice: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Senior Dimensions: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Smart Choice/Nevada Check Up: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Sierra Health and Life: |
|
|
Out of plan |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Sierra Spectrum: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Phone: (LV) 702-242-7330 (outside LV) 800-288-2264 |
|
|
Requesting Provider Name: |
Fax #: (LV) 702838-8297 (outside LV) 888-633-9301 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Date of Request: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Member Name & member number: |
|
|
|
|
|
|
|
Requesting Provider’s Address & Phone #: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Requesting Provider’s Fax #: |
|
|
|
|
|
|
|
|
|
|
Members Address & Phone #: |
|
|
|
|
|
|
|
Requesting Provider’s Tax ID #: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
HIPAA Provider Identification #: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Member’s DOB: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Contact Person (Name, Phone & Fax # :) |
|
|
|
|
|
|
|
|
|
|
Employer Group’s Name & Phone #: |
|
|
|
|
|
|
|
Requesting Provider’s Signature or Stamped Signature: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Other Insurance(s): |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Diagnosis (incl. ICD code): |
|
|
|
|
|
|
|
Procedure/Treatment Request (incl. CPT code): |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Number of Treatments Requested: ______________ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Inpatient / Outpatient: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Services Requested by Patient: YES NO |
|
|
|
|
|
|
|
|
|
|
Service Provider / Address / Phone #: |
|
|
|
|
|
|
|
Place of Service / Facility and Address: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Requested Procedure Date / Start Treatment Date: |
|
|
|
|
|
|
|
|
Area for internal health plan use only |
|
|
Authorization: |
|
|
|
|
|
Date of Authorization: |
Pended / Denied: (Reason): |
CURRENT CLINICAL FINDINGS AND |
MANAGEMENT |
|
use the space – also see requirements below and attach to this form. |
All procedures/treatment requested require |
clinical information (may |
Health Plan Contact name & phone #: |
|
|
Yes |
|
No |
Authorization Number: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
*All sections of this form must be completed.
Pertinent Attachments=Information to support the proposed diagnosis, treatment/procedure; i.e. current clinical findings (progress reports), results
of laboratory testing, imaging studies (x-rays, etc.) must be submitted to prevent processing delays.
**On adverse determinations a reconsideration / expedited appeal may be requested.
* All Sections of this form must be completed.
**On adverse determinations a reconsideration / expedited appeal may be requested.
This referral/authorization is not a guarantee of payment. Payment is contingent upon eligibility, benefits available at the time the service is rendered, contractual terms, limitations, exclusions, and coordination of benefits, and other terms & conditions set forth in the member’s Evidence of Coverage, Certificate of Coverage, or Self Insured Employer’s Plan Documents.
The information contained in this form, including attachments, is privileged and confidential & is only for the use of the individual or entities named on this form. If the reader of this form is not the intended recipient or the employee or the agent responsible to deliver to the intended recipient, the reader is hereby notified that any dissemination, distribution, or copying of this communication is strictly prohibited. If this communication has been received in error, the reader shall notify sender immediately and shall destroy all information received.
Revised 2/24/16
S4590 (02/16)